Standing in the pharmacy aisle in front of 20 different prenatal vitamins – all claiming to be the best – is one of the most quietly overwhelming moments of trying to conceive. Here’s the truth: most of them are more similar than they look. What actually matters is whether they contain the right nutrients, in the right forms, at the right doses.
Once you know what those are, the choice becomes much clearer.
This guide covers the 7 nutrients that matter most in a prenatal vitamin, when to start taking them before pregnancy, how to read a label confidently, and what common pitfalls to avoid – including why a regular multivitamin is not an adequate substitute.
One important note: prenatal vitamins are designed to supplement a healthy diet, not replace it. DHA (from fatty fish or algae), calcium (from dairy, leafy greens, or fortified foods), and choline (from eggs) are nutrients your prenatal may only partially cover – and that’s intentional. If you have specific health conditions, a history of pregnancy complications, or dietary restrictions, talk to your doctor or midwife before choosing – this guide is a starting point, not a prescription.

When Should You Start Taking Prenatal Vitamins?
The standard medical recommendation is to begin at least one to three months before you start trying to conceive. Some healthcare providers suggest starting as early as three to six months prior for maximum benefit1.
Here’s why the timing matters so much: your baby’s brain and spinal cord begin forming within the first 21-28 days of fetal development – often before you’ve even gotten a positive pregnancy test. By the time most women know they’re pregnant, this critical developmental window has already opened.
Folic acid in particular needs time to build to protective levels in your body, which is why starting preconception – months before a positive test – can make a real difference in outcomes.
If you find out you’re pregnant and haven’t been taking prenatal vitamins yet, start them immediately. And if you’re in a situation where individual guidance matters – which we’ll cover later in this article – your doctor is the right first stop.
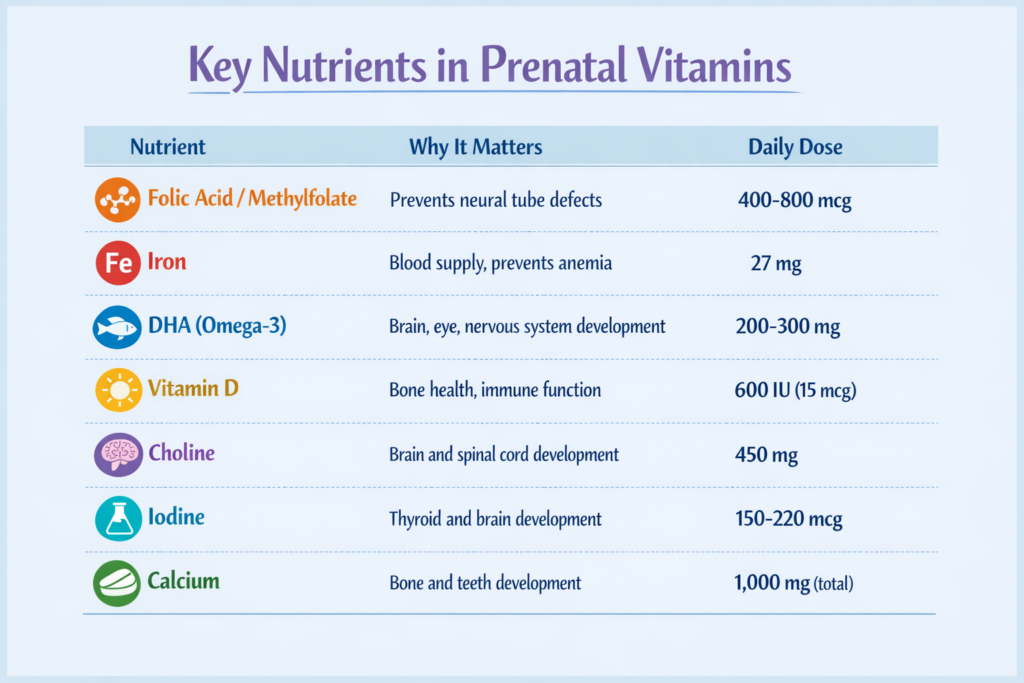
7 Essential Nutrients to Look for in a Prenatal Vitamin
These are the non-negotiables – the nutrients with the strongest evidence for preconception and early pregnancy health. If any of the situations described below the nutrient list apply to you, individual guidance from your doctor will serve you better than any general recommendation.
1. Folic Acid – The Most Important One
Folic acid (vitamin B9) is the single most studied and critical nutrient in prenatal supplementation. Adequate intake in the preconception period reduces the risk of neural tube defects (NTDs) – serious birth defects affecting the brain (anencephaly) and spinal cord (spina bifida) – by up to 70%2.
Recommended dose: 400-800 mcg per day for most people trying to conceive. If you have had a previous pregnancy affected by an NTD or carry an MTHFR gene variant, your doctor may prescribe 4,000 mcg (4 mg) – do not take this higher dose without medical guidance.
Folic acid vs. methylfolate: Folic acid is the synthetic form of vitamin B9. Your body must convert it into its active form (methylfolate / 5-MTHF) to use it. Up to 60% of people carry a common MTHFR gene variant that impairs this conversion3. If you’re in that group, a prenatal containing methylfolate (also labelled L-methylfolate or 5-MTHF) may be more beneficial. Many newer prenatal vitamins now offer methylfolate or a combination of both forms.
2. Iron
Iron supports the growth of the placenta and fetus, and helps your body produce the extra blood volume pregnancy requires. Inadequate iron is one of the most common causes of pregnancy-related anemia4.
Recommended dose: 27 mg per day (higher than the standard adult recommendation of 18 mg).
Practical note: Iron is the most common cause of prenatal vitamin side effects – nausea, constipation, and stomach discomfort. Taking your prenatal with a small amount of food helps, as does evening dosing if morning nausea is a problem. Iron and calcium compete for absorption, so if you take additional calcium supplements, space them apart by a few hours.
3. DHA (Omega-3 Fatty Acid)
DHA (docosahexaenoic acid) supports your baby’s brain, eye, and nervous system development – particularly during the third trimester. It may also support egg quality before conception.
Recommended dose: At least 200-300 mg per day. Not all prenatal vitamins include DHA – check the label. Eating 2 servings per week of low-mercury fish (salmon, sardines, trout) is also a well-supported way to meet your DHA needs alongside supplementation.
Source matters: DHA can come from fish oil (look for “molecularly distilled” or “mercury-tested”) or algae – equally effective and suitable for those avoiding fish.
4. Vitamin D
Vitamin D works in partnership with calcium for bone development and plays a role in immune function and reducing the risk of pregnancy complications.
Recommended dose: 600 IU (15 mcg) per day as a baseline. Vitamin D deficiency is very common, particularly in northern latitudes. Ask your doctor for a blood test if you suspect deficiency – you may need a higher supplemental dose.
5. Choline
Choline is essential for your baby’s brain and spinal cord development, yet many prenatal vitamins still don’t include adequate amounts.
Recommended dose: 450 mg per day. Eggs are a particularly accessible dietary source – if your prenatal contains 200-300 mg of choline, food can close the gap easily.
6. Iodine
Iodine is critical for thyroid hormone production and supports your baby’s brain and nervous system development throughout pregnancy.
Recommended dose: 150-220 mcg per day5. Check your prenatal label – iodine is still absent from some formulations. Those following dairy-free or vegan diets may have lower dietary iodine than expected.
7. Calcium
If your calcium intake is insufficient, your body draws from your own bone stores to supply the fetus.
Recommended total intake: 1,000 mg per day from prenatal and diet combined. Most prenatals don’t include the full amount (calcium is bulky), so make up the difference through dairy, fortified plant milks, leafy greens, or a separate supplement. This is completely normal – no single prenatal pill is designed to be your only source of calcium.
At a glance:
For broader preconception preparation beyond nutrition – including cycle tracking, sleep, and timing – see the guide on how to increase your chances of getting pregnant naturally.
Prenatal Vitamin vs. Regular Multivitamin – Is There a Difference?
Yes – and it matters for safety, not just completeness.
Prenatal vitamins are formulated specifically for the increased nutritional demands of supporting new life: higher doses of folic acid, iron, and usually DHA are standard6.
The most important distinction is vitamin A. Many regular adult multivitamins contain preformed vitamin A (listed as “retinol” or “retinyl palmitate”) – which at high doses can be harmful during pregnancy and the preconception period. Prenatal vitamins use beta-carotene instead, which the body converts to vitamin A only as needed.
Bottom line: A regular multivitamin is not an adequate substitute for a prenatal during the preconception period or pregnancy. If you’re trying to conceive, switching to a dedicated prenatal is the right move.
How to Read a Prenatal Vitamin Label
Third-party testing certifications
Look for seals from: USP, NSF International, GMP, or Consumer Lab. These verify purity and label accuracy – the most important single quality signal on any supplement.
Bioavailable forms
- Folate: look for methylfolate, L-methylfolate, or 5-MTHF (or at minimum, folic acid)
- B12: methylcobalamin is more bioavailable than cyanocobalamin
Vitamin A source
Must list beta-carotene – not retinol, not retinyl palmitate.
DHA source
“Algae-derived” suits those avoiding fish. Fish-oil DHA should be “molecularly distilled” or “mercury-tested.”
Avoid mega-dosing
100-150% of the RDA for most nutrients is appropriate. 500-1000% is not – especially for fat-soluble vitamins A, D, E, and K.
Common Side Effects and How to Manage Them
The most common complaint is iron-related: nausea, constipation, or stomach discomfort.
Helpful strategies:
- Take your prenatal with a small amount of food, not on an empty stomach
- Switch to evening dosing if morning nausea is a problem
- Some providers suggest splitting into two doses per day (morning and evening) to reduce GI side effects
- Drink plenty of water and eat fibre-rich foods throughout the day
- Give your body 2-4 weeks to adjust before switching products
If nausea persists, gummy prenatals may be better tolerated – but most gummies don’t contain iron, so check the label. Low-iron and iron-free formulations also exist and may suit those who aren’t deficient. Your OB or midwife can advise based on your iron levels.
Alongside starting your prenatal, how to track ovulation at home is a practical next step in preconception preparation.
![A warm photo of a woman talking with a healthcare provider in a bright, approachable clinic setting]](https://babiesparent.com/wp-content/uploads/2026/02/A-warm-photo-of-a-woman-talking-with-a-healthcare-provider-in-a-bright-approachable-clinic-setting.jpg)
When to Talk to Your Doctor Before Choosing a Prenatal
For most people, any reputable third-party-tested prenatal with folic acid (400-800 mcg), 27 mg iron, DHA, and vitamin D is a solid choice. But these situations call for a conversation first:
- Previous pregnancy affected by a neural tube defect: May need prescribed 4 mg (4,000 mcg) folic acid
- Known or suspected MTHFR gene variant: Methylfolate formulation may be recommended
- Thyroid conditions: Iodine supplementation needs individual monitoring
- Vegetarian or vegan diet: Confirm iron, B12, and algae-derived DHA levels
- Difficulty swallowing pills: Liquid, chewable, and gummy formulations exist
- Taking other medications: Disclose your prenatal to your prescriber – interactions are possible
Frequently Asked Questions
Can I take a prenatal vitamin if I’m not yet pregnant?
Yes – this is the whole point. Prenatal vitamins are specifically designed to be started preconception, not only after a positive test. They are safe and beneficial to take before pregnancy.
Is it safe to take prenatal vitamins when trying to conceive?
Yes. The key caution is to avoid high doses of preformed Vitamin A (retinol) – which is why a dedicated prenatal using beta-carotene is preferable to a regular multivitamin during this period.
What’s the difference between folic acid and folate in prenatal vitamins?
Folic acid is the synthetic form of vitamin B9 that must be converted by the body into its active form (methylfolate). Up to 60% of people have an MTHFR variant that impairs this conversion. Methylfolate (5-MTHF) can be used by the body directly. Both are found in prenatal vitamins; those with MTHFR variants may benefit from a methylfolate-containing formula.
Do prenatal vitamins help you get pregnant?
Not directly, but they support the nutritional conditions for conception. For the full picture of conception strategies, see the guide on how to increase your chances of getting pregnant naturally.
What happens if I forgot to take my prenatal vitamin?
Missing one day is not a problem. Continue with your regular dose the next day – do not double up.
Can prenatal vitamins cause nausea?
Yes, particularly the iron component. Taking your prenatal with food, switching to evening doses, or splitting into two doses per day can help. If symptoms persist, speak with your healthcare provider about alternatives7.
Final Thoughts
Starting prenatal vitamins before pregnancy is one of the most impactful, evidence-backed steps you can take on the road to conception. The goal isn’t finding a perfect pill – it’s making sure that when the time comes, your body has what it needs.
Prioritize folic acid or methylfolate, iron, DHA, and vitamin D. Choose a product with third-party certification. Confirm the Vitamin A source is beta-carotene. Start at least one to three months before you begin trying.
If you have specific health needs, your doctor or midwife is the right person to make it personal.
You’re doing exactly the right thing by researching this now.
- Cleveland Clinic – Prenatal Vitamins: Purpose, Types and When to Start, https://my.clevelandclinic.org/health/drugs/22734-prenatal-vitamins
- KidsHealth / Nemours – Folic Acid and Pregnancy, https://kidshealth.org/en/parents/folic-acid.html
- BabyCenter – Methylfolate vs Folic Acid in Prenatal Vitamins, https://www.babycenter.com
- Mayo Clinic – Prenatal vitamins: Why they matter, how to choose, https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/prenatal-vitamins/art-20046945
- NHS UK – Vitamins, supplements and nutrition in pregnancy, https://www.nhs.uk/pregnancy/keeping-well/vitamins-supplements-and-nutrition/
- WebMD – What Should You Look for in a Prenatal Vitamin?, https://www.webmd.com/baby/what-should-you-look-for-in-a-prenatal-vitamin
- WebMD – What Should You Look for in a Prenatal Vitamin?, https://www.webmd.com/baby/what-should-you-look-for-in-a-prenatal-vitamin