If your doctor has mentioned IUI or IVF as next steps, you’re probably trying to figure out what each one actually involves – and whether there’s a meaningful difference between them. There is. Here’s what you need to know before your next appointment.
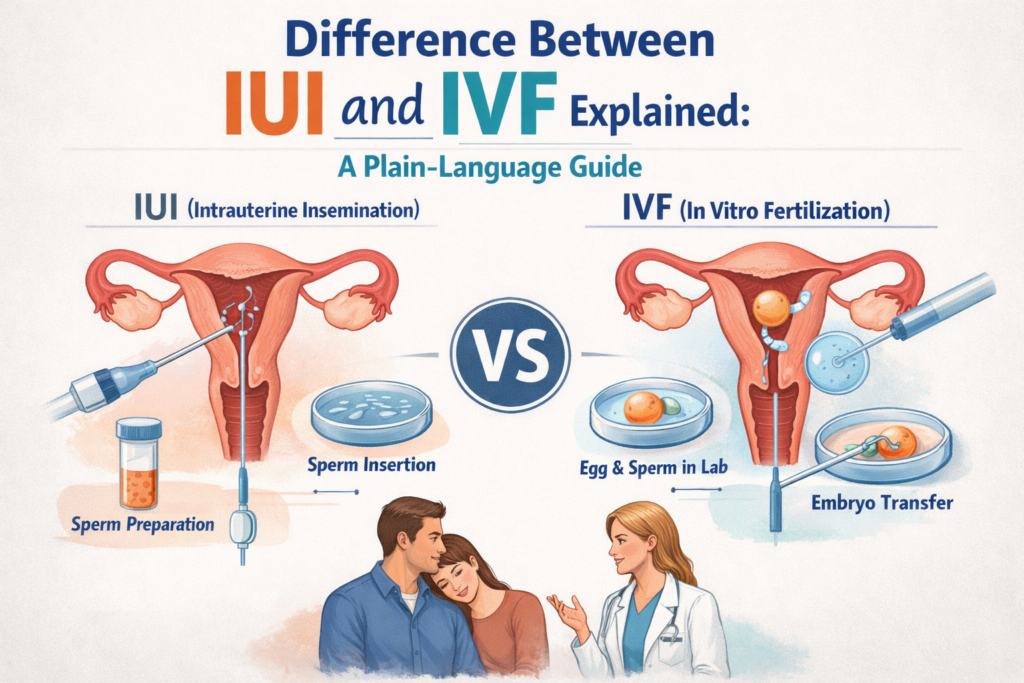
IUI (Intrauterine Insemination) places prepared sperm directly inside the uterus so fertilization can still happen naturally inside the body. IVF (In Vitro Fertilization) retrieves eggs from the body, fertilizes them in a laboratory, and places the resulting embryo back into the uterus.
These are two very different procedures – different in invasiveness, cost, success rates, and which fertility challenges each can address. Neither is inherently “better.” They are tools for different situations. A reproductive endocrinologist can help determine which is right for your specific diagnosis.
What Is IUI? How It Works
In short: washed sperm is placed inside the uterus, shortening the distance to the egg. Fertilization still happens naturally in the fallopian tube. Takes about 10 minutes, no anesthesia required.
The IUI Process – Step by Step
1. Ovarian stimulation (optional but common)
Low-dose oral medications (Clomid/letrozole) or injectable gonadotropins stimulate the ovaries to mature one to three eggs. IUI can be done in a natural cycle, but stimulation improves success rates.
2. Monitoring
Regular ultrasounds and blood tests track follicle growth and hormone levels to ensure correct timing.
3. Trigger shot
When follicles reach the right size, an hCG trigger shot is given. This induces ovulation in approximately 36 hours, allowing the clinic to time the insemination precisely.
4. Sperm collection and washing
A sperm sample is collected and sent to the lab for sperm washing – a process that isolates the healthiest, most motile sperm from seminal fluid, dead sperm, bacteria, and debris. Seminal plasma contains prostaglandins that can cause severe uterine cramping if injected directly into the uterus; sperm washing removes these before insemination, making the procedure safe.
5. Insemination
A thin, flexible catheter is passed through the cervix and the washed sperm is deposited directly into the uterus. The procedure takes 5-10 minutes and is similar to a Pap smear. No anesthesia is required. Mild cramping is possible afterward.
6. Pregnancy test
You rest briefly and resume normal activity. A pregnancy test is taken approximately two weeks later.
Total timeline: approximately one menstrual cycle (4 weeks) per attempt.
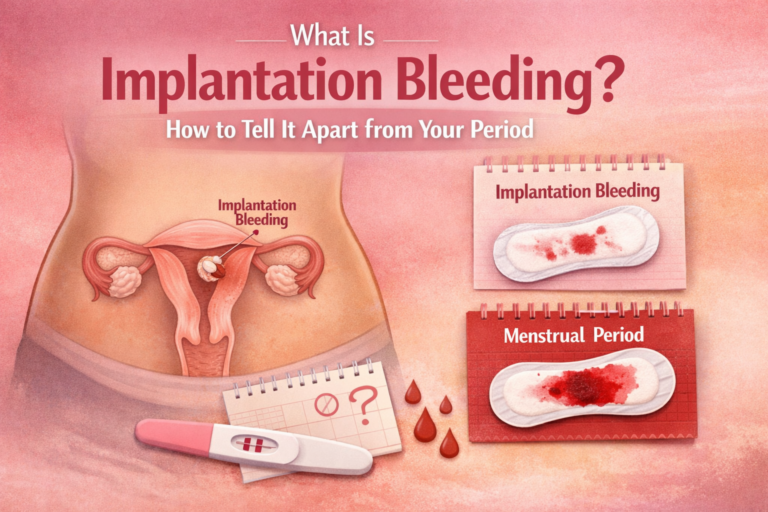
Understanding your cycle timing is important for IUI success. See: how to track ovulation at home.
What Is IVF? How It Works
In short: eggs are retrieved from the ovaries, fertilized in a laboratory, and the resulting embryo is placed into the uterus. Because fertilization happens outside the body, IVF works even when fallopian tubes are blocked or sperm quality is very poor.
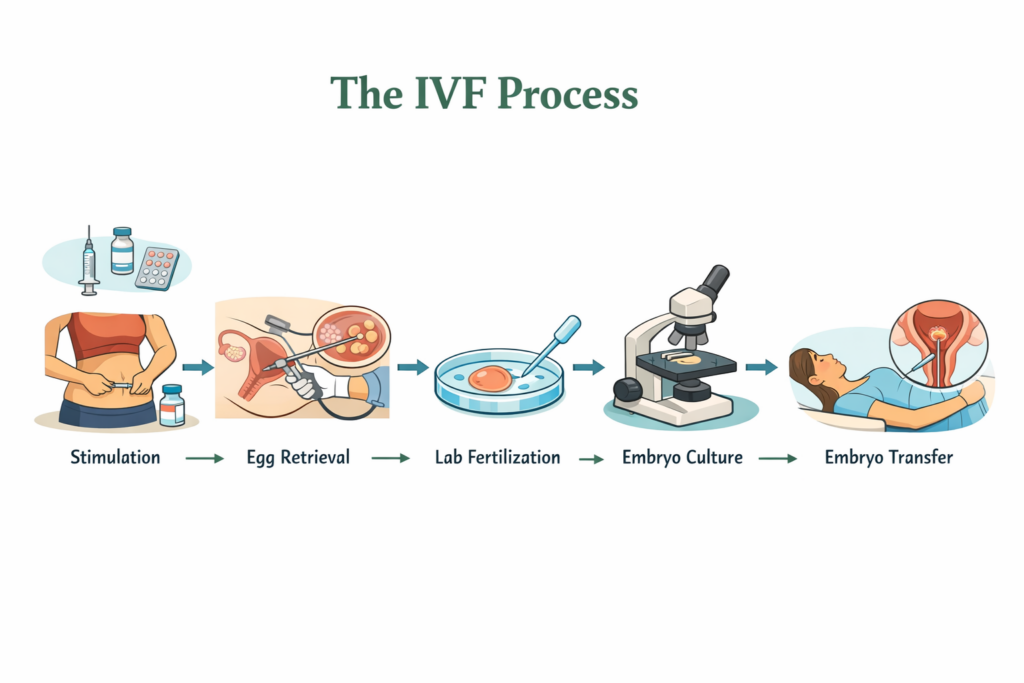
The IVF Process – Step by Step
1. Ovarian stimulation
Daily hormone injections (8-14 days) stimulate the ovaries to produce multiple mature eggs – typically 8-15, compared to 1-3 in IUI. More eggs give the lab more opportunities to create viable embryos.
2. Monitoring
Frequent ultrasounds and blood tests every 2-3 days track follicle development. IVF requires significantly more clinic appointments than IUI.
3. Trigger shot
Administered 34-36 hours before egg retrieval to finalize egg maturation.
4. Egg retrieval
A minor surgical procedure under sedation. An ultrasound-guided needle passes through the vaginal wall into each ovarian follicle to aspirate the egg. Takes 15-30 minutes. Patients go home the same day. Some tenderness and bloating for 1-2 days afterward is normal.
5. Fertilization in the laboratory
Retrieved eggs and prepared sperm are combined. Two methods:
- Standard IVF: Eggs and sperm are placed in a dish together and fertilization occurs naturally in the lab
- ICSI (Intracytoplasmic Sperm Injection): A single sperm is injected directly into each egg. Used when sperm quality is very low, or when previous IVF cycles had poor fertilization rates. Now used in the majority of IVF cycles globally.
6. Embryo culture
Fertilized eggs are monitored in the lab for 3-6 days as they develop into embryos. The goal is for embryos to reach the blastocyst stage (day 5-6) before transfer or freezing.
7. Preimplantation Genetic Testing – PGT (optional)
Before transfer, embryos can be screened for chromosomal abnormalities. Recommended for women over 38, those with recurrent pregnancy loss, or couples who are carriers of genetic conditions. Genetically normal embryos have higher implantation rates and lower miscarriage risk1.
8. Embryo transfer
One embryo is placed into the uterine cavity via catheter under ultrasound guidance. Takes 5-10 minutes. No anesthesia typically needed. Remaining viable embryos can be frozen for future transfer cycles (FET – frozen embryo transfer).
9. Pregnancy test
Approximately two weeks after transfer.
Total timeline: approximately 4-6 weeks per full IVF cycle.
IUI vs IVF – The Key Differences at a Glance
| Feature | IUI | IVF |
|---|---|---|
| Where fertilization happens | Inside the body (fallopian tube) | Outside the body (laboratory) |
| Invasiveness | Minimal (like a Pap smear) | Moderate (daily injections + minor surgery) |
| Anesthesia | Not required | Required for egg retrieval (sedation) |
| Cycle duration | ~4 weeks | ~4-6 weeks |
| Clinic appointments per cycle | ~4-6 | ~10-15 |
| Success rate per cycle (under 35) | 10-20% | 50-65% |
| Cost per cycle (approx.) | $300-$4,000 | $10,000-$25,000 |
| Works with blocked fallopian tubes | No | Yes |
| Works with severe male factor infertility | No | Yes (with ICSI) |
| Embryo freezing possible | No | Yes |
| Genetic embryo screening (PGT) | No | Yes |
Sources: SART, RMA Network, Cleveland Clinic
The table gives you the technical picture. Now let’s talk about the human one: which situation typically calls for which treatment.
Who Is Each Treatment Right For?
IUI Is Typically Recommended When…
- Mild male factor infertility – moderately low sperm count, reduced motility, or mild morphology issues; sperm washing and direct uterine delivery compensate for mild deficiencies
- Unexplained infertility – when no specific cause has been identified; IUI is usually the first treatment tried
- Cervical factor – cervical mucus hostility or scarring that impedes sperm from passing through the cervix naturally
- Ovulatory dysfunction – irregular or absent ovulation; typically combined with ovulation-induction medication
- Mild endometriosis – when tubes are not severely involved
- Donor sperm use – for single women, same-sex couples, or couples where one partner has no viable sperm
- When a lower-cost, less invasive first step is medically appropriate
IUI will not be effective when:
- Fallopian tubes are blocked or severely damaged – sperm still cannot reach the egg
- Sperm count is very low or motility is near-zero even after washing
- Moderate or severe endometriosis with tubal involvement
IVF Is Typically Recommended When…
- Blocked or damaged fallopian tubes – IVF bypasses the tubes entirely; fertilization occurs in the lab2
- Severe male factor infertility – IVF with ICSI can achieve fertilization with very few sperm, including surgically retrieved sperm
- After 3-6 failed IUI cycles – when IUI has not worked after multiple attempts
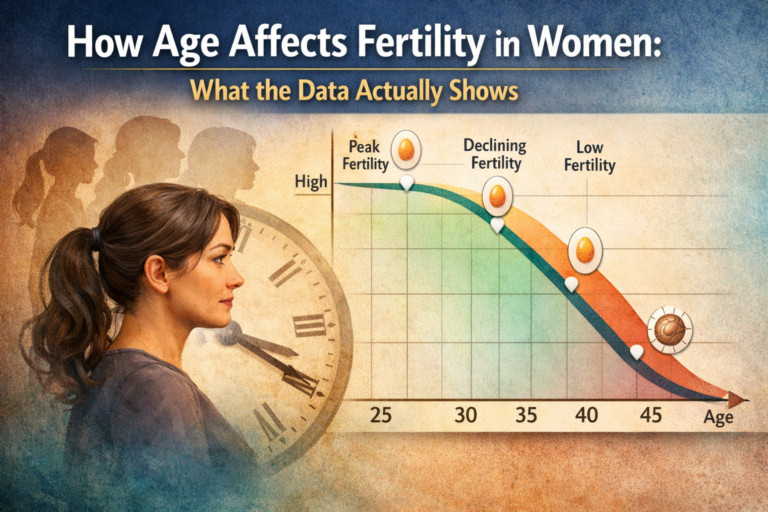
- Advanced maternal age – IVF offers higher per-cycle success rates where fertility is more significantly declined. See: how age affects fertility in women
- Diminished ovarian reserve – retrieving multiple eggs maximizes the number of viable embryos
- Moderate or severe endometriosis involving the tubes or ovaries
- Preimplantation Genetic Testing (PGT) needed – recurrent pregnancy loss, chromosomal carrier status, advanced age
- Reciprocal IVF – for same-sex female couples; one partner’s eggs, the other carries
Success Rates and Costs – What to Expect
Success Rates by Age
IUI – approximate live birth rates per cycle:
- Under 35: ~10-20%
- 35-40: ~5-10%
- Over 40: ~2-5%
- Cumulative over 3-4 cycles (under 37): approximately 40-50%
IVF – approximate live birth rates per cycle (SART national data, own eggs):
- Under 35: ~50-65%
- 35-37: ~40-50%
- 38-40: ~25-35%
- Over 40 (own eggs): ~10-20%
- Over 44 (own eggs): <5%3
For women over 44 using their own eggs, success rates with IVF are low. However, donor egg IVF can achieve live birth rates of 40-50%+ per cycle regardless of the recipient’s age – because success depends on the donor’s egg quality rather than the recipient’s ovarian age. This is an important option for many women in this group.
For couples under 37 with open tubes and mild fertility factors, starting with 3 IUI cycles is often medically and financially appropriate. For women over 38, or those with blocked tubes, severe male factor, or other complex factors, moving directly to IVF is usually recommended.
Cost Breakdown
IUI:
- Per cycle: $300 – $4,000
- Add oral medications: +$30-75
- Add injectable medications: +$100-2,000
- Typical 3-cycle investment: $1,500 – $6,000+
IVF:
- Per cycle (monitoring + retrieval + fresh transfer): $10,000 – $25,000
- Medications: +$2,000 – $7,000
- PGT (if done): +$3,000 – $6,000
- Frozen embryo transfer (FET): +$3,000 – $5,000
Insurance coverage varies widely. In the US, coverage depends on state law and employer plan. In the UK, NHS funding may be available under specific criteria. Many fertility clinics offer financing plans – ask your clinic what options are available. Always confirm your coverage with your insurer and clinic before beginning4.
Note: while IVF costs more per cycle, its higher success rates mean fewer cycles needed on average. For some couples, the total treatment cost over time may not differ as dramatically as the per-cycle comparison suggests.
Frequently Asked Questions
What is the main difference between IUI and IVF?
The core difference is where fertilization occurs. In IUI, sperm is placed inside the uterus and fertilization happens naturally inside the body (in the fallopian tube). In IVF, eggs are retrieved from the ovaries and fertilized in a laboratory; the resulting embryo is then placed into the uterus.
Is IVF more painful than IUI?
IUI involves minimal discomfort – mild cramping similar to a Pap smear, no anesthesia. IVF involves daily injections (bruising and soreness are common) and egg retrieval under sedation. Most patients find egg retrieval well-tolerated, with some bloating and tenderness for 1-2 days. IVF is more physically demanding, but not typically described as severely painful.
Can IVF work after multiple failed IUI cycles?
Yes. IUI and IVF work differently, and failed IUI does not predict IVF failure. Many people who experience multiple failed IUI cycles go on to have successful pregnancies through IVF5.
How many IUI cycles should you try before moving to IVF?
Most fertility specialists recommend 3-6 IUI cycles before moving to IVF, assuming you are under 38, have open fallopian tubes, and no other specific reasons to escalate sooner. For women over 38, your reproductive endocrinologist may recommend moving to IVF earlier.
Does IVF work for blocked fallopian tubes?
Yes – this is one of the primary indications for IVF. Because fertilization occurs in the lab and the embryo is placed directly into the uterus, blocked or absent fallopian tubes do not prevent IVF from working.
Is IUI or IVF more expensive overall?
IVF costs more per cycle ($10,000-$25,000+ vs. $300-$4,000 for IUI). However, IVF’s significantly higher per-cycle success rate means fewer cycles needed on average. For some couples, the cumulative total of multiple IUI cycles versus one effective IVF cycle may be closer than the per-cycle comparison suggests.
What is ICSI, and how does it differ from regular IVF?
ICSI (Intracytoplasmic Sperm Injection) is a variation of IVF in which a single sperm is injected directly into each egg, rather than leaving sperm and eggs to fertilize in a dish. ICSI is used when sperm quality is very poor, or when previous IVF cycles resulted in poor fertilization. It’s now used in the majority of IVF cycles worldwide and does not significantly affect success rates compared to standard IVF when used appropriately.
Final Thoughts
IUI and IVF are not competing treatments – they’re different solutions for different situations. IUI is less invasive, lower-cost, and appropriate for many couples with mild fertility factors and open tubes. IVF is more involved and more expensive, but it offers significantly higher success rates and addresses challenges IUI cannot.
The fertility journey carries its own emotional weight, and knowing what each step involves makes it possible to navigate it with clearer eyes. For more on how stress and the emotional side of fertility treatment interconnect, see how stress affects fertility.
The most important next step is a thorough conversation with a reproductive endocrinologist who can evaluate your specific situation and recommend the right starting point for you.
- Mayo Clinic – In Vitro Fertilization (IVF), https://www.mayoclinic.org/tests-procedures/in-vitro-fertilization/about/pac-20384716
- Shady Grove Fertility – IUI vs IVF, https://www.shadygrovefertility.com/blog/treatments-and-success/iui-vs-ivf/
- SART – IVF Success Rates, https://www.sart.org/patients/a-patients-guide-to-assisted-reproductive-technology/general-information/in-vitro-fertilization-ivf/
- Cleveland Clinic – IUI Process, https://my.clevelandclinic.org/health/treatments/22096-intrauterine-insemination-iui
- Advanced Fertility Center – IUI vs IVF, https://www.advancedfertility.com/iuivsivf.htm