If one more person tells you to “just relax and it’ll happen,” you might scream. It’s the most frustrating thing to hear when you’re trying to conceive. And yet – here’s the uncomfortable truth – the science behind that advice isn’t entirely wrong.
Chronic stress really does affect your reproductive hormones. Not in a vague, hand-wavy way, but through a specific biological pathway that can suppress ovulation, reduce sperm quality, and make conception genuinely harder.
But there’s an important distinction most people miss: it’s chronic stress – the sustained, grinding kind – that causes hormonal disruption, not the everyday stress of a full life. And more importantly, there are real, evidence-backed things you can do about it.
This article explains the mechanism clearly, covers how stress affects both female and male fertility, addresses the painful feedback loop that TTC creates, and gives you a practical toolkit of stress-reduction strategies with actual research behind them.
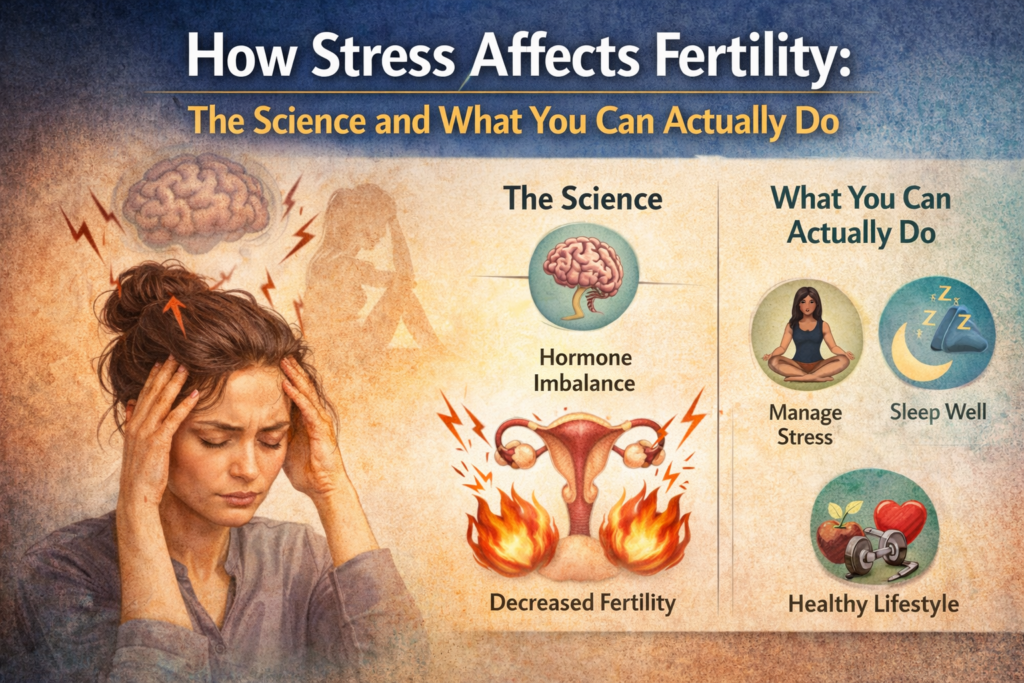
The Science: How Stress Hormones Interfere with Reproduction
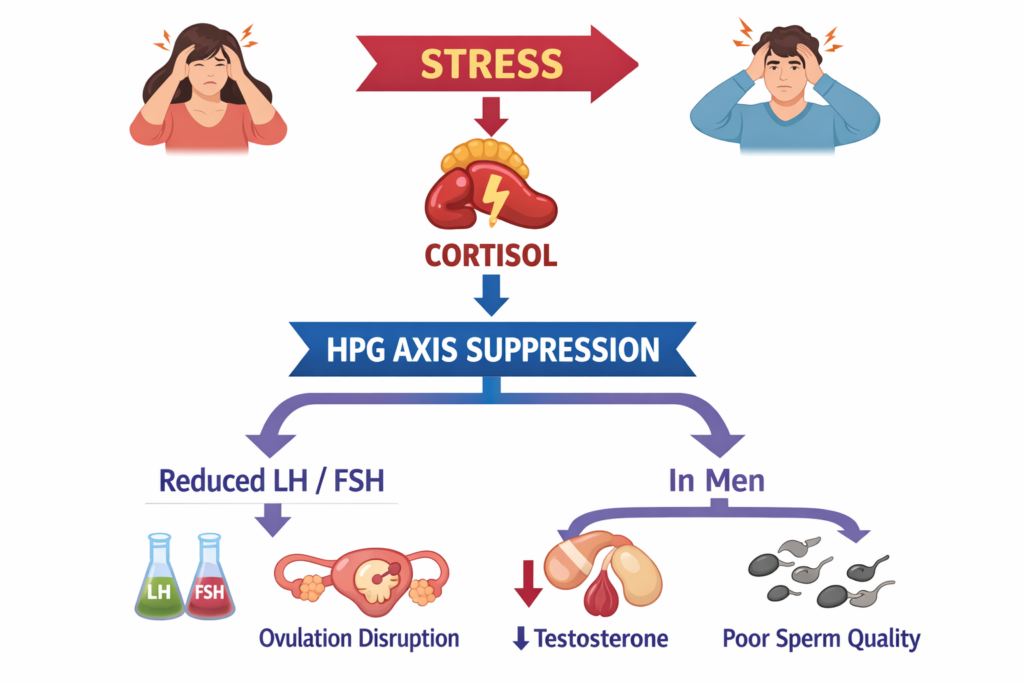
To understand why stress affects fertility, you need to know about one pathway: the HPG axis (Hypothalamic-Pituitary-Gonadal axis). Think of it as your body’s reproductive chain of command.
Under normal conditions: your hypothalamus (brain) sends a signal via GnRH (gonadotropin-releasing hormone – the starter signal) to your pituitary gland, which releases FSH (follicle-stimulating hormone, which matures follicles in the ovaries) and LH (luteinizing hormone, which triggers the release of the egg). These hormones travel to the ovaries or testes and coordinate ovulation and sperm production respectively.
When you’re chronically stressed, your body floods the system with cortisol – the primary stress hormone. Cortisol is essentially an interceptor on this chain of command. It suppresses GnRH at the hypothalamus, which means the pituitary doesn’t receive the signal it needs to release LH and FSH – and without those hormones, both ovulation and sperm production are compromised1.
Cortisol also directly suppresses estrogen and progesterone – the sex hormones that regulate the menstrual cycle and support early pregnancy.
The key word throughout all of this is “chronic.” A stressful week, an intense month, or even a particularly hard season is unlikely to derail your fertility on its own. The concern is sustained, ongoing stress that keeps cortisol elevated over a long period of time.
How Stress Affects Female Fertility
For women, the most direct consequence of elevated cortisol is disruption to ovulation.
Irregular or suppressed ovulation: Cortisol can inhibit the LH surge that triggers egg release. Without that LH surge, ovulation doesn’t happen – and if ovulation doesn’t happen, neither does a period, leading to the cycle irregularities that many women under sustained stress begin to notice. A 2022 meta-analysis found that women experiencing high stress were 30% more likely to report menstrual irregularities than lower-stress controls2.
Longer time to conception: A 2023 longitudinal study found that women reporting high psychological stress took a 40% longer time to conceive compared to women with lower stress levels. That’s a meaningful, clinically significant difference.
Egg quality and implantation: Chronically elevated cortisol reduces estradiol, the estrogen responsible for egg maturation. It may also impair the uterine lining (endometrium), potentially making implantation harder. Women with higher chronic cortisol levels – measured from hair samples in one research design – showed lower pregnancy rates after IVF.
Preconception impact: A 2024 NIH study found that maternal stress immediately before conception was negatively associated with the probability of a live birth, particularly for women undergoing IVF3. This reinforces why the period before you start trying matters, not just the months during.
When stress disrupts ovulation, the signals your body normally sends around fertile days can become harder to read. Paying attention to the signs of ovulation you should not ignore becomes particularly important – and more challenging – during high-stress periods.
How Stress Affects Male Fertility
The conversation about stress and fertility tends to focus on women. But the evidence for male impact is just as significant – and too often overlooked.
Testosterone and sperm production: Cortisol suppresses testosterone – the hormone that drives spermatogenesis (the process of sperm development from production to maturation). When testosterone drops, sperm count typically follows4. Research from Columbia University found that men with elevated cortisol produced sperm with lower motility, abnormal morphology, and reduced overall count5.
Oxidative stress and DNA damage: Beyond count and motility, chronic psychological stress generates oxidative stress in semen. This cellular-level stress damages the DNA inside sperm cells – affecting not just fertilization rates but embryo quality and early pregnancy outcomes.
Reduced sex drive: Chronically low testosterone from sustained cortisol exposure also reduces libido – which can, practically speaking, reduce the frequency of intercourse at key points in the fertile window.
According to the American Psychological Association, stress is a contributing factor in up to 50% of male infertility cases6 – a statistic that makes clear why male fertility needs to be fully included in this conversation.
The encouraging part: Sperm are produced continuously in a cycle of about 72-74 days. This means that improvements in stress levels and lifestyle habits show up in semen quality within roughly 2-3 months – a meaningful window if you have an upcoming fertility appointment or are early in treatment. Unlike egg reserve (which is fixed), sperm quality is genuinely and measurably improvable.
The Feedback Loop: When Infertility Becomes the Stressor
Here’s the most difficult part of the stress-fertility relationship to talk about: infertility itself generates profound stress.
Research has found that the psychological burden of infertility can be comparable to a cancer diagnosis – and yet couples are often expected to manage this quietly while continuing to perform medically timed intercourse, track every ovulation signal, and remain hopeful month after month7.
The result is a feedback loop: trying to conceive creates stress; that stress elevates cortisol; elevated cortisol disrupts the hormones needed to conceive; which means conception takes longer; which increases anxiety further.
This cycle is not a personal failure. It’s a physiological reality – and naming it matters, because it’s the reason stress management is a legitimate, evidence-based part of a fertility plan, not just gentle advice to take a bubble bath and calm down.
Being gentle with yourself during this process isn’t weakness. It’s science.
What Actually Helps: Evidence-Based Stress Reduction Strategies
These techniques are listed because they have research behind them – not because they’re easy or guaranteed, but because they’ve been specifically studied in relation to fertility and stress.
Mindfulness and Meditation
Mindfulness practices – even brief, simple ones – meaningfully reduce cortisol levels and psychological distress in women with infertility. In a randomized controlled study, 52% of women in a structured mind-body program conceived and delivered successfully, compared to just 20% in the control group8. Even 10 minutes of guided meditation daily – via apps like Calm, Headspace, or free YouTube resources – can shift cortisol patterns over weeks.
Yoga
Yoga combines movement, breathwork, and meditation – all three reduce cortisol independently. Restorative yoga in particular activates the parasympathetic “rest and digest” nervous system, directly counteracting the cortisol-driven stress state. For male partners: research suggests yoga may reduce DNA fragmentation in sperm, giving it value for both people in the TTC partnership.
Acupuncture
Acupuncture is one of the more extensively studied complementary therapies in fertility care. It significantly reduces stress markers, and some studies suggest it may also support ovulation through nervous system modulation and increased ovarian blood flow, and potentially improve IVF outcomes9. Evidence is moderate rather than definitive, but its safety profile is excellent alongside conventional fertility treatments.
Therapy and Cognitive Behavioral Therapy (CBT)
CBT breaks the anxiety spiral that infertility creates and has a strong evidence base for reducing health-related anxiety and cortisol. If TTC has begun to affect your relationship, your self-image, or your daily functioning, a therapist experienced in infertility is one of the highest-impact investments you can make. Couples counseling can also reduce the joint stress that the process puts on a partnership.
Sleep
Cortisol rises significantly with sleep deprivation – so poor sleep directly feeds the hormonal disruption this article describes. Aim for 7-9 hours per night, with consistent bedtime and wake times. This is often the fastest, most underestimated change people can make.
Moderate Exercise
Regular moderate movement (walking, swimming, cycling, light strength training) reduces baseline cortisol and supports hormonal balance. The caveat: excessive high-intensity exercise can suppress ovulation in women who are already lean. Keep it consistent and moderate.
Social Support
Infertility remains a largely private struggle, and isolation amplifies its weight. Finding even one or two people you can be fully honest with – a close friend, a trusted family member, or an online TTC community – makes a measurable difference in emotional resilience.
As effective as these strategies are, they work best as part of a larger fertility plan. For the full picture – including timing, nutrition, and lifestyle factors – see the guide on how to increase your chances of getting pregnant naturally.

What Stress Management Won’t Do – and When to See a Doctor
This is important, and worth saying clearly: stress management is a supportive measure, not a cure for structural infertility.
Many causes of fertility challenges – blocked fallopian tubes, endometriosis, polycystic ovary syndrome (PCOS), low ovarian reserve, azoospermia, significant sperm abnormalities – have nothing to do with stress levels. Reducing stress will not resolve these conditions.
Use these timelines as your guide for when to seek a professional evaluation:
- Under 35: See a doctor after 12 months of regular unprotected sex
- Ages 35-39: See a doctor after 6 months
- Over 40: Don’t wait – seek an evaluation right away
- Any age: Seek evaluation sooner if you have irregular cycles, PCOS, endometriosis, a history of miscarriage, or a partner with known sperm concerns
A medical evaluation is not a failure. It’s information – and information is what moves you forward.
If you’re unsure whether you’re ovulating consistently, tracking your ovulation at home is a practical first step that gives you real data to bring to that first appointment.
Frequently Asked Questions
Can stress actually stop you from getting pregnant?
Chronic, sustained stress can suppress ovulation, disrupt the menstrual cycle, and reduce sperm quality – making conception harder. It’s one factor among many, rarely the sole cause of infertility, but a real physiological factor with solid research behind it.
How much stress is too much for fertility?
The critical distinction is chronic stress vs. everyday stress. A difficult week or even a hard month is unlikely to derail fertility on its own. Sustained elevation of cortisol over months or years drives hormonal disruption. If stress is affecting your sleep, your cycle, or your overall functioning, it’s worth actively addressing.
Can stress cause a missed period?
Yes – this is one of the most documented effects. Elevated cortisol can suppress the LH surge that triggers ovulation. Without ovulation, menstruation doesn’t follow. At the extreme end, this is called “hypothalamic amenorrhea” – a condition where chronic stress (or extreme exercise or severe calorie restriction) halts the cycle entirely. Milder cortisol elevation can cause delays or irregular timing.
Does stress affect IVF success?
Research suggests that higher chronic cortisol is associated with lower pregnancy rates in IVF, and that preconception stress is negatively associated with live birth outcomes. The relationship is complex – many patients conceive despite high stress – but managing stress during treatment is a legitimate, medically supported goal.
What is the fastest way to reduce stress when trying to conceive?
The techniques with the clearest evidence are mindfulness, yoga, and acupuncture. But the single fastest, most overlooked change is consistent sleep: 7-9 hours per night at regular times directly lowers cortisol. Start with whatever feels most accessible and sustainable for you.
Final Thoughts
The stress-fertility connection is real – and more specific than “just relax.” Cortisol disrupts the hormonal cascade your body needs to ovulate reliably, mature eggs, produce testosterone, and develop healthy sperm. Chronic stress is a genuine fertility headwind, for both partners.
But you’re not powerless here. Mindfulness, yoga, acupuncture, therapy, sleep, and moderate exercise all have evidence behind them. You don’t need to do all of them. Pick one that resonates and build from there.
Just don’t add “reducing stress” to the list of things you’re anxious about. The goal is a lighter load – not another performance standard.
And if you’re at the 6-month or 12-month mark without success, reach out to your doctor. That conversation is the most empowering next step – stress levels and all.
- NIH – Stress and Female Reproductive Function, https://pubmed.ncbi.nlm.nih.gov/12428682
- Frontiers in Psychology – Stress, cortisol and infertility, https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1017924
- NIH – Preconception stress and live birth probability, https://www.nih.gov/news-events/news-releases
- NIH – Psychological stress and sperm quality, https://pubmed.ncbi.nlm.nih.gov/11477519
- Columbia University – Stress and male fertility, https://www.columbia.edu
- APA – Stress effects on male reproductive health, https://www.apa.org
- Cleveland Clinic – Stress and Infertility, https://my.clevelandclinic.org/health/diseases/22191-infertility
- Denver Fertility Care – Mind-body program outcomes, https://denverfertilitycare.com
- NIH – Acupuncture mechanisms in fertility, https://pubmed.ncbi.nlm.nih.gov/22464950