Your tests came back normal. His tests came back normal. And yet – nothing. “Unexplained infertility” is one of the harder diagnoses to receive, not because it’s the most serious, but because it gives you nothing to fix. Here’s what it actually means, what it may be missing, and where to go from here.
Unexplained infertility is a diagnosis given when all standard fertility tests for both partners return within the normal range, yet pregnancy has not occurred after 12 months of trying – or six months if you’re over 35. Standard tests confirm ovulation, check fallopian tube patency, review uterine structure, assess ovarian reserve, and analyze the male partner’s sperm. When all of those come back normal, the result is this particular diagnosis.
About 1 in 5 infertile couples receive it – some estimates put the range at 10-30%1. And the most important number to know right at the start: up to 92% of couples with unexplained infertility ultimately have a child with appropriate treatment and time2. That doesn’t make receiving this diagnosis easy. But it does mean there is a real, well-traveled path forward.
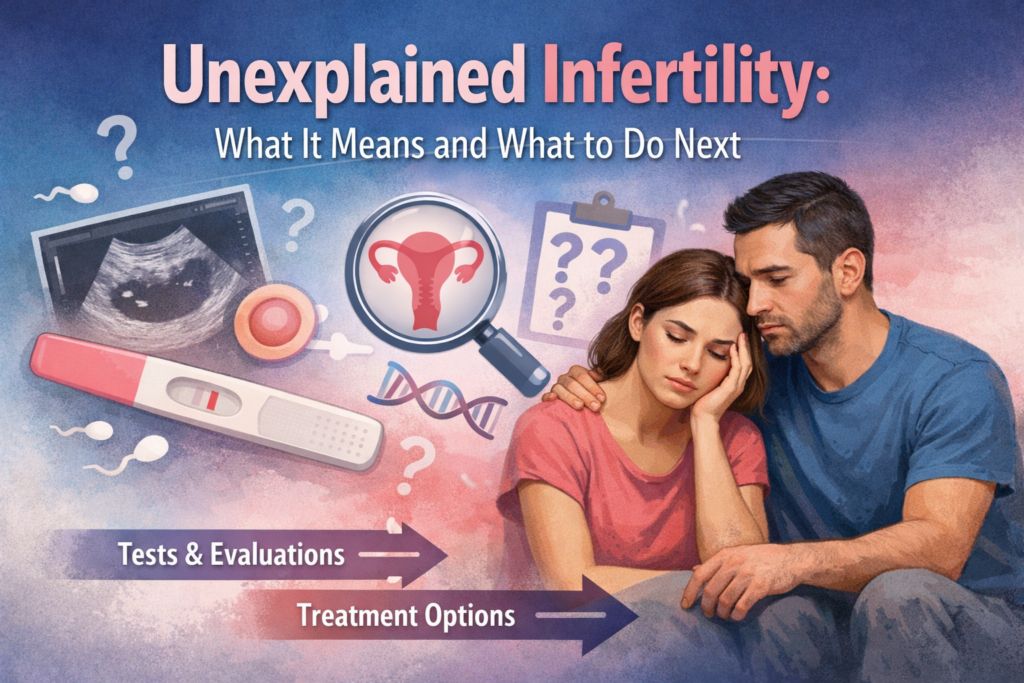
What “Unexplained Infertility” Actually Means
It’s a Diagnosis of Exclusion – Not a Diagnosis of Nothing
“Unexplained infertility” does not mean nothing is wrong. It means that what is wrong has not yet been identified by the standard diagnostic tests.
Think of it like a car that won’t start but returns no error codes on any diagnostic scan. The car is still not starting. The problem is real – it’s simply below the level that standard instruments can detect.
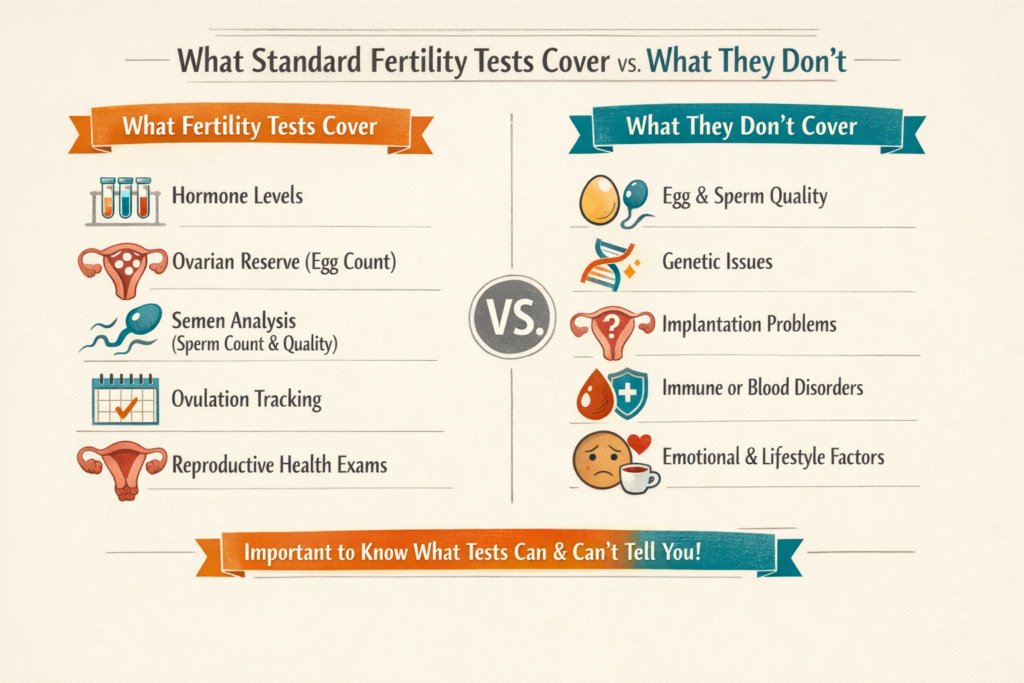
The standard fertility workup rules out the most common and identifiable causes: major ovarian reserve issues, blocked fallopian tubes, significant structural problems, and severe semen abnormalities. Ruling these out is genuinely useful information. But fertility involves extraordinarily complex biological interactions – at the cellular and molecular level – that standard tests don’t yet capture.
“Unexplained” describes the current limit of the test battery. It does not describe the limit of your situation.
Why This Diagnosis Feels So Hard
With most fertility diagnoses – blocked tubes, low sperm count, anovulation – there’s a specific target. Treatment addresses that target.
With unexplained infertility, there’s no specific target. Which makes treatment feel less like solving a problem and more like casting wide nets. Research has found that couples with unexplained infertility can experience higher psychological distress than those with clearly identified diagnoses – because ongoing uncertainty is its own kind of burden3.
This frustration is completely normal. And the fact that the standard workup is complete does not mean your options are limited.
Can You Still Conceive Naturally?
Studies suggest that up to 43% of couples with unexplained infertility conceive naturally without any medical intervention – particularly within the first 2-3 years of trying. For couples under 35 with no additional risk factors, a period of “expectant management” – continuing to try naturally while implementing lifestyle optimization – for up to 2 years from the initial diagnosis is a legitimate medical approach.
However, age changes this calculation meaningfully. As egg quality declines with age, the window for natural conception narrows. For women approaching or over 35, being proactive sooner is generally the right call.
Expectant management is not giving up. It’s an active, informed choice made with medical guidance, based on your age, how long you’ve been trying, and your overall health picture.
What Standard Tests May Have Missed
Standard tests rule out the most common identifiable causes. Several factors, however, go beyond the standard diagnostic toolkit – none of these mean your previous workup was inadequate; they simply represent areas worth exploring further with your specialist.
Egg Quality
There’s a critical distinction between egg quantity and egg quality. Tests like AMH (Anti-Mullerian Hormone) and antral follicle count assess how many eggs remain. They say nothing about how good those eggs are.
Egg quality refers to chromosomal integrity – whether an egg can fertilize and develop into a viable embryo. Poor egg quality can look like: fertilization that fails even when sperm reach the egg, an embryo that stops developing after day 2-3 in the lab, or a very early pregnancy loss (sometimes called a “chemical pregnancy”) before 6 weeks. These patterns provide important diagnostic information – and are only visible through an IVF cycle, when eggs are retrieved and fertilization is attempted.
Age is the most significant driver of egg quality decline, and how age affects fertility in women follows a steeper curve than most people expect. But egg quality problems can occur in younger women independently of age as well.
Sperm DNA Fragmentation
A standard semen analysis checks sperm count, motility, and morphology. It does not check the genetic integrity of the DNA inside each sperm cell.
Sperm DNA fragmentation refers to breaks or damage in the DNA strands within a sperm. Sperm with high fragmentation may fertilize an egg – but the resulting embryo may fail to develop properly, or implant briefly and then miscarry. High fragmentation is associated with recurrent pregnancy loss and failed IVF cycles even when all other semen parameters appear normal.
Causes include oxidative stress, infections, smoking, excessive alcohol, heat exposure to the testes, and advanced paternal age. A specific sperm DNA fragmentation test (not included in standard semen analysis – must be ordered separately) can measure this. And importantly: fragmentation is often improvable. An antioxidant protocol – CoQ10, vitamin C, vitamin E, zinc, selenium – taken consistently for at least 3 months (the time needed for a complete sperm production cycle of 72-90 days) can meaningfully reduce fragmentation levels.
Silent Endometriosis
Endometriosis is a condition where tissue similar to the uterine lining grows outside the uterus. “Silent” endometriosis produces no obvious symptoms – no painful periods, no pelvic pain. Many women have it for years without any indication.
It still affects fertility. Silent endometriosis creates a chronic inflammatory environment that can damage egg quality and disrupt embryo implantation. It is not visible on ultrasound or HSG. The only reliable way to diagnose it is laparoscopy – a minor surgical procedure where a camera directly examines the pelvic cavity.
If you have any pelvic or period pain that hasn’t been fully explored, it’s worth asking your specialist whether laparoscopy is appropriate.
Endometrial Receptivity
Even when the uterine lining appears normal on ultrasound, it may not be optimally receptive to an embryo at the right moment. Think of it as a door that’s only open for a specific 12-24 hour window each cycle. The ERA test (Endometrial Receptivity Array) – a precisely timed biopsy of the uterine lining – determines exactly when your window opens.
This test is primarily relevant within an IVF cycle, particularly if you’ve had failed embryo transfers with good-quality embryos. Less applicable to natural conception or IUI.
Immune Factors (Investigational)
The immune system plays a role in tolerating a pregnancy – allowing the embryo (which is genetically “foreign”) to implant. In some cases, immune dysfunction may interfere with this.
Factors being studied include overactive natural killer (NK) cells, antithyroid antibodies, and antiphospholipid antibodies. Immune-based fertility treatment remains more investigational – clinics vary significantly in their approach. Not a first-line area to explore, but worth discussing if other approaches haven’t worked.
Your Next Steps: A Clear Path Forward
Step 1: Optimize What You Can Control
Start here regardless of your treatment plan. These changes can meaningfully improve outcomes – particularly sperm DNA quality, which is frequently overlooked.
For both partners:
- Quit smoking: directly damages egg DNA and increases sperm DNA fragmentation
- Limit alcohol: affects egg quality and multiple sperm parameters
- Maintain a healthy body weight: affects ovulation, egg quality, and sperm production
For her:
- Start a prenatal vitamin with methylfolate (not just folic acid – some people cannot convert folic acid efficiently)
- Check your vitamin D levels – deficiency is common and linked to fertility outcomes
- Moderate, regular exercise – but not excessive; very high training loads can disrupt ovulation
For him:
- Antioxidant protocol: CoQ10 (200-600mg/day), vitamin C (1000mg), vitamin E (400IU), zinc, selenium – maintain for at least 3 months, as a full sperm production cycle takes 72-90 days to complete
- Reduce heat exposure to the testes: no laptops on your lap, avoid hot baths and saunas, switch to looser underwear
On stress: Chronic stress activates the HPA (hypothalamic-pituitary-adrenal) axis, which runs through the same hormonal pathways that regulate reproduction – which is how stress affects fertility in a measurable, not just psychological, way. Managing it is worth pursuing for this specific physiological reason.
Step 2: Ask About Additional Testing
These are not included in every standard workup:
- Sperm DNA fragmentation test – relevant if semen analysis is borderline, or after recurrent early losses or failed IVF cycles
- Laparoscopy – to definitively rule out endometriosis, especially with pelvic or period pain
- Hysteroscopy – direct examination inside the uterine cavity; detects small polyps or fibroids missed on standard ultrasound
- ERA test – within IVF context, if failed transfers with good embryos
- Extended immune panel – antithyroid and antiphospholipid antibodies – particularly relevant with recurrent pregnancy loss
If your diagnosis came from a general OB/GYN, requesting a referral to a reproductive endocrinologist (RE) is a reasonable step. REs see unexplained infertility regularly and can guide the additional testing conversation.
Step 3: Medical Treatment by Age
| Age | Recommended Starting Point |
|---|---|
| Under 35 | Ovulation induction + timed intercourse (3 cycles), then IUI with stimulation (3-6 cycles), then IVF |
| 35-37 | IUI with stimulation (3-6 cycles), with active discussion of moving to IVF sooner |
| 38 and over | IVF directly – preserves time and maximizes egg retrieval |
IUI success rates (unexplained infertility):
- Natural cycle IUI: ~7-10% per cycle
- IUI + Clomid/letrozole: ~8% per cycle
- IUI + injectable FSH: ~12% per cycle
- Cumulative over 3 cycles (under 37): approximately 15-25%4
IVF success rates (unexplained infertility):
- Under 35: ~40-50% per cycle
- 35-37: ~30-40%
- 38-40: ~20-30%
- Over 40: ~5-15%5
A key advantage of IVF is that the cycle itself provides diagnostic information IUI cannot – fertilization rates, embryo development quality, and whether quality patterns explain prior failures. Understanding the difference between IUI and IVF – how they work, what each cycle involves, and what each can reveal – helps you have a more informed conversation with your RE about which to prioritize.
The Emotional Side – What No One Tells You
Unexplained infertility carries a particular emotional difficulty. Being told “everything looks normal” when you know something isn’t working can feel disorienting – even, at times, like not being believed. That experience is real and widely shared.
Research has found that couples with this diagnosis can experience more distress than those with a known cause – because when there’s a specific diagnosis, there’s at least something to address. Uncertainty carries its own weight.
What unexplained infertility is not:
- Not “in your head”
- Not “just relax and it will happen” – stress matters biologically, but it is not the root cause
- Not a sign that something is unsolvably wrong
It is: a recognized diagnosis with well-documented treatment pathways and strong overall outcomes. Up to 92% of couples who pursue appropriate care have a child.
Both partners carry this diagnosis emotionally. The male partner’s experience is often more quietly carried and less often acknowledged. Support together is more effective than support alone.
Practical next steps for support:
- Ask your clinic if they have a fertility counsellor or social worker – many do
- RESOLVE (resolve.org) – National Infertility Association, with peer support networks, forums, and local groups
- Individual or couples therapy with a therapist who specializes in fertility or medical stress
Frequently Asked Questions
What does unexplained infertility mean?
It means all results in the standard fertility testing battery – for both partners – came back within the normal range, but pregnancy has not occurred. It’s a “diagnosis of exclusion.” The most common identifiable causes have been ruled out. It does not mean nothing is wrong; it means the cause has not been detected by current standard testing.
What are the hidden causes of unexplained infertility?
The most commonly missed factors include: egg quality issues (standard tests measure quantity, not quality), sperm DNA fragmentation (not assessed in standard semen analysis), silent endometriosis (only diagnosable via laparoscopy), and suboptimal endometrial receptivity (assessable via ERA test in IVF cycles). Immune factors are also studied, though more investigational.
Can you get pregnant naturally with unexplained infertility?
Yes. Up to 43% of couples with unexplained infertility conceive naturally without medical treatment, particularly within the first 2-3 years. For women under 35, expectant management (watchful waiting with lifestyle optimization) for up to 2 years is a legitimate medical approach. For women over 35, being proactive sooner is generally advisable.
Should I try IUI or go straight to IVF?
It depends on age. Under 35: IUI (3-6 cycles) is a reasonable starting approach. Ages 35-38: discuss the timeline trade-off with your RE. Over 38: most specialists recommend IVF directly – it offers higher per-cycle success rates and preserves time.
How many IUI cycles should I try before moving to IVF?
Most specialists recommend 3-6 IUI cycles before moving to IVF, assuming you are under 38 with open fallopian tubes. Some move to IVF after 3 unsuccessful cycles for women over 356.
What tests should I ask about if I have unexplained infertility?
If not yet done: sperm DNA fragmentation test, laparoscopy if endometriosis symptoms are present, hysteroscopy to examine the uterine cavity. In an IVF context with failed transfers: ask about the ERA test. With recurrent pregnancy loss: ask about an extended immune panel.
Does stress cause unexplained infertility?
Stress is not a root cause. “Just relax” is frustrating advice because it implies you could simply think your way to pregnancy. However, chronic stress activates the HPA axis, which does intersect with the hormonal pathways governing reproduction. Stress management is worth pursuing for its specific physiological effects – alongside proper medical investigation and treatment.
Where to Go from Here

Unexplained infertility is not a dead end. It is an incomplete picture – and medicine has developed clear, evidence-based ways to fill in the gaps.
Start with what you can control: lifestyle changes that improve egg and sperm quality take at least 3 months to show results, so beginning that process now runs in parallel with whatever clinical path you pursue. Request any missing tests – particularly sperm DNA fragmentation and, if endometriosis is at all possible, laparoscopy. And if you’ve been working with a general OB/GYN, a consultation with a reproductive endocrinologist is worth pursuing – REs see this diagnosis regularly and can offer a structured plan based on your specific age, timeline, and history.
The most useful thing to hold onto: up to 92% of couples with this diagnosis ultimately have a child with appropriate care. The path is less certain than with a named diagnosis, but it is well-traveled, and you are not at its end.
- NIH / NCBI – Unexplained Infertility, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5865535/
- Cleveland Clinic – Unexplained Infertility, https://my.clevelandclinic.org/health/diseases/17778-unexplained-infertility
- RESOLVE – Unexplained Infertility, https://resolve.org/learn/what-is-infertility/unexplained-infertility/
- Advanced Fertility Center – IUI Success Rates, https://www.advancedfertility.com/iuivsivf.htm
- SART – Clinic Summary Report, https://www.sart.org
- ASRM – Unexplained Infertility, https://www.asrm.org/globalassets/asrm/asrm-content/news-and-publications/practice-guidelines/for-non-members/unexplained_infertility.pdf